Turkish Nobel scientist Aziz Sancar’s brain cancer breakthrough enters human trials
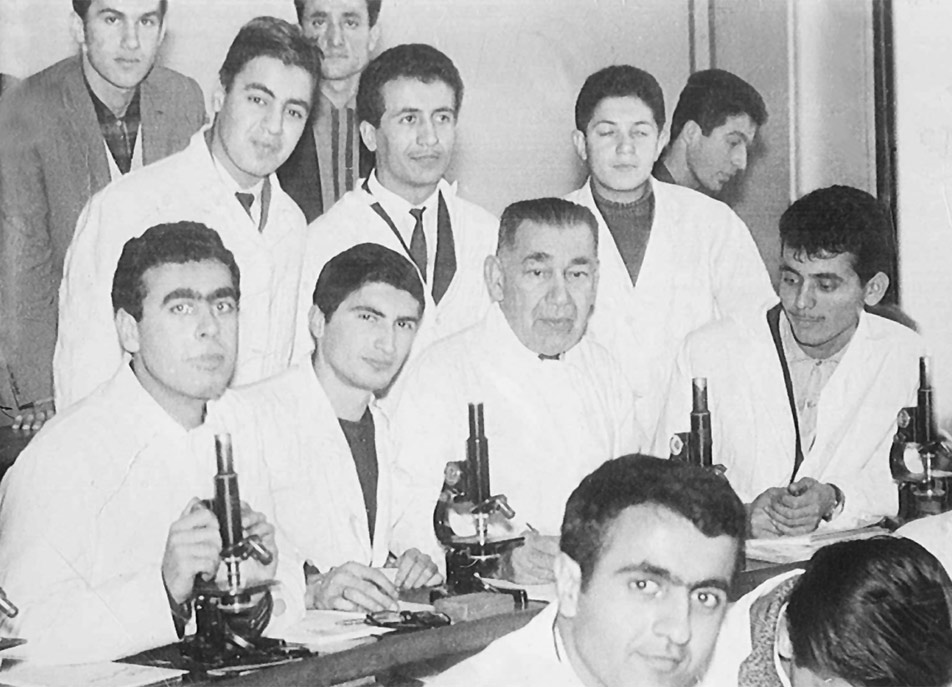
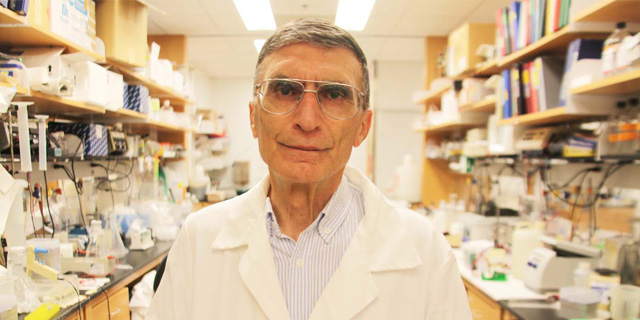
 Aziz Sancar gives a speech at Istanbul University, Türkiye, May 29, 2016. (Shutterstock Photo)
Aziz Sancar gives a speech at Istanbul University, Türkiye, May 29, 2016. (Shutterstock Photo)
Nobel Prize-winning scientist professor Dr. Aziz Sancar’s revolutionary research into brain cancer treatment is now entering the critical stage of human trials.
After years of successful laboratory and animal testing by the Turkish Nobel scientist Aziz Sancar and his team, the next phase will study the effects of the EdU molecule in humans over two years.
This development brings hope for new, effective treatments against one of the most challenging forms of cancer.

Sancar first introduced his research on Feb. 17, 2022, calling it an “exciting discovery.” Since then, his team has focused on how EdU, a molecule commonly used in molecular biology, could treat brain tumors by targeting cancerous cells more effectively than existing treatments.
Aziz Sancar explained that the molecule they discovered “enters the brain easily and kills cancer cells.”
Turkish Nobel scientist Aziz Sancar to offer new hope for brain cancer patients
Sancar’s research centers on the EdU molecule, which has the ability to cross the blood-brain barrier – a natural defense that has hindered many cancer treatments. The widely used cancer drug Cisplatin, for example, cannot penetrate this barrier and is therefore ineffective in treating brain tumors.
Sancar pointed out that current cancer drugs are “ineffective in treating this type of cancer because they cannot pass the blood-brain barrier.”
What makes EdU stand out is its ability to not only pass through this barrier but also to selectively kill fast-dividing cancer cells while sparing healthy ones. Sancar explained that “EdU can kill rapidly dividing cancerous brain cells while protecting non-dividing healthy brain cells,” highlighting the potential of this molecule as a breakthrough in brain cancer treatment.
The research process involved working with various neuroscience departments. The team created realistic brain cell models by placing human brain tumor samples into slices of mouse brains.
After injecting the tumors into the mouse brains, the team observed how EdU affected them. Initially, traditional cancer drugs outperformed EdU, but after 30 to 40 days, EdU surpassed them in effectiveness. When combined with existing drugs, “the results were even better,” Sancar noted.
Human trials are the next major step in this brain cancer research
Following the success of the animal trials, Sancar’s team is moving forward with human testing. Over the next two years, they will focus on assessing EdU’s side effects and ensuring it can replicate the same level of effectiveness seen in animal models.
In his statement, Aziz Sancar emphasized that “we need to study its side effects in humans for two years before it can be used.”
Sancar also expressed his desire to share the results of his research with Türkiye. His efforts to transfer this technology to the country reflect his ongoing commitment to advancing scientific discoveries globally.
If these trials prove successful, EdU could become a game-changer in the treatment of brain cancer, offering new hope for patients who currently have limited options.



